Mild Cognitive Impairment: Early Signs You Shouldn’t Ignore
It starts small.
You forget where you left your keys. You walk into a room and can’t remember why. You struggle to recall the name of a colleague you’ve worked with for years. These moments can be brushed off as “normal aging,” and often they are. But sometimes, they’re not.
These could be early signs of Mild Cognitive Impairment (MCI)—a condition that affects thinking and memory, and may be a warning sign of something more serious.
Let’s unpack what MCI is, why early detection matters, and which signs you (or your loved ones) should pay close attention to.
What Is Mild Cognitive Impairment (MCI)?
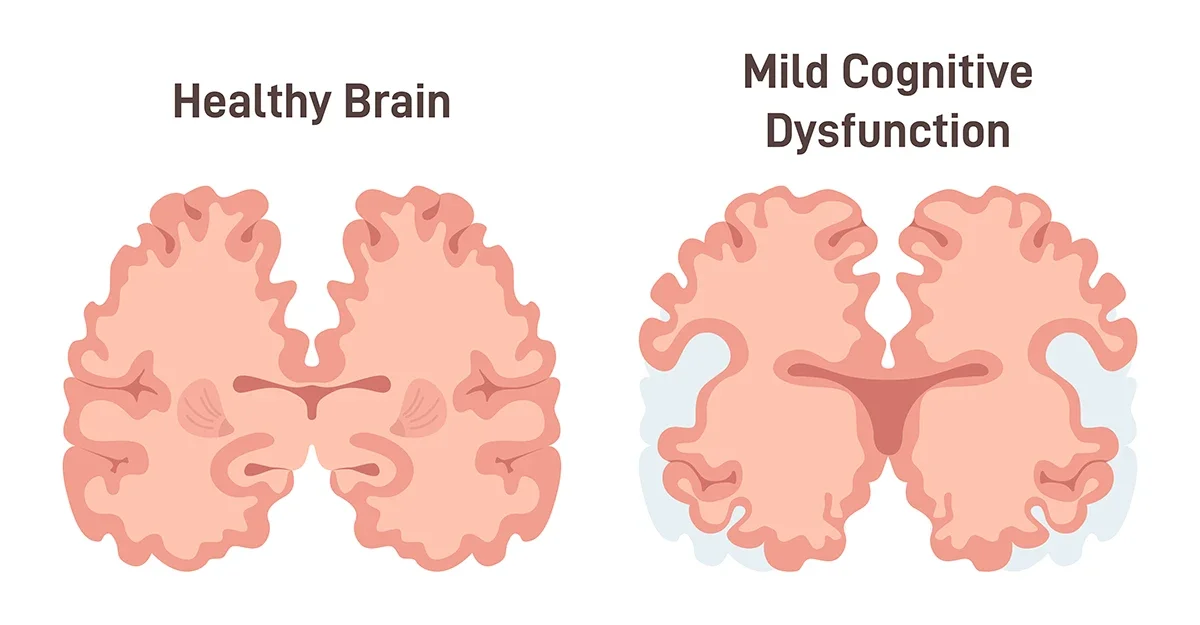
Mild Cognitive Impairment is a noticeable, measurable decline in cognitive abilities—like memory and thinking—that’s greater than expected for your age, but not severe enough to interfere significantly with daily life or independence.
In other words: you’re functioning, but something feels “off.” You or others may notice a change, and it's more than just “senior moments.”
MCI is often a middle ground between typical age-related memory loss and more serious conditions like Alzheimer’s disease or other types of dementia.
Two Types of MCI
Understanding the specific type of Mild Cognitive Impairment (MCI) is key to choosing the right therapy, monitoring changes, and supporting daily life. MCI is generally categorized into two types: amnestic and non-amnestic.
Amnestic MCI primarily affects memory. People with this type may frequently forget recent conversations, misplace items, miss appointments, or ask the same questions repeatedly. These memory lapses go beyond typical age-related forgetfulness and are noticeable enough to raise concern, though they don’t yet interfere significantly with daily independence.
Non-amnestic MCI, on the other hand, impacts other cognitive skills. This might include problems with decision-making, visual perception (like judging distances or navigating spaces), attention and concentration, or language — such as struggling to find the right words or follow the flow of a conversation. While memory may remain mostly intact, these other cognitive disruptions can still affect daily functioning and quality of life.
Recognizing which type of MCI is present can help doctors tailor treatment approaches, whether that involves cognitive therapy, lifestyle changes, or closer monitoring for progression.
Early Signs You Shouldn’t Ignore
Not every memory lapse points to cognitive decline, but a pattern of subtle changes can signal a problem worth checking. Here are signs that may indicate Mild Cognitive Impairment:
1. Memory Loss That’s Noticeable to Others
Everyone forgets names or dates from time to time. But with MCI, the forgetfulness becomes consistent and noticeable, even to people around you.
You might:
Ask the same questions repeatedly
Forget important dates or events
Struggle to retain new information
2. Trouble Following Conversations
You might find yourself getting lost mid-conversation or struggling to keep up in group discussions.
This could look like:
Frequently asking “What did you say?”
Losing your train of thought
Difficulty understanding jokes or metaphors
3. Difficulty with Routine Tasks
Tasks you used to handle effortlessly—paying bills, managing appointments, cooking familiar meals—start to feel overwhelming or confusing.
It’s not about being careless. It’s about feeling mentally foggy or unsure of steps you’ve done a hundred times before.
4. Poor Judgment or Decision-Making
You might make choices that seem uncharacteristic:
Over- or under-tipping at restaurants
Falling for phone scams
Making impulsive purchases
These small shifts can indicate changes in executive functioning, which controls planning, judgment, and reasoning.
5. Decreased Sense of Direction
Getting lost on the way to familiar places—or struggling to follow a map or GPS—is another red flag.
Spatial awareness often declines early in cognitive conditions.
6. Changes in Mood or Personality
MCI can also come with subtle emotional shifts:
Increased anxiety or irritability
Depression or apathy
Withdrawal from social activities or hobbies
These aren’t just emotional responses—they may be early neurological signs of cognitive decline.
How Is MCI Diagnosed?
Diagnosing Mild Cognitive Impairment isn’t based on a single test — it involves a comprehensive look at a person’s cognitive function, daily habits, and overall health. The process typically begins with a detailed medical history, including any self-reported changes in memory, thinking, or attention. Often, input from family members or close friends is also crucial, since loved ones may notice subtle changes that the person themselves may overlook or downplay.
From there, healthcare providers will conduct standardized cognitive assessments that evaluate memory, attention span, problem-solving skills, language use, and the ability to plan or organize. These tests help determine if a person’s cognitive performance is below what’s expected for their age and education level.
To rule out other possible causes of memory problems — like a vitamin deficiency, thyroid imbalance, stroke, or depression — doctors may also recommend neurological exams, brain imaging (such as MRI or CT scans), and blood work. These tests help ensure that symptoms aren’t being caused by something treatable or unrelated to cognitive decline.
If you're concerned about your memory or that of someone you care about, the most important step is to talk to a healthcare provider. Catching the signs of MCI early gives you more choices for managing symptoms, planning for the future, and possibly slowing progression — especially if it’s related to a condition like Alzheimer’s that benefits from early intervention.
Is Mild Cognitive Impairment Reversible?
Mild Cognitive Impairment (MCI) isn’t always a one-way path to dementia — and in many cases, it can be stabilized or even improved, especially when the underlying cause is identified and treated. While MCI is often associated with early stages of Alzheimer’s or other neurodegenerative conditions, it can also stem from reversible or manageable issues. Common treatable causes include sleep disorders like sleep apnea, vitamin B12 deficiencies, depression, certain medications, thyroid imbalances, and even chronic stress or anxiety. When these contributing factors are properly addressed, many individuals see noticeable improvements in memory, focus, and overall cognitive function. That’s why early evaluation is so important — not all MCI cases are permanent or progressive, and getting to the root of the symptoms can lead to better outcomes and peace of mind.
How Can Speech-Language Therapy Help?
When people hear “speech therapy,” they often think of pronunciation or stuttering. But speech-language pathologists (SLPs) also specialize in cognitive-communication therapy—helping individuals strengthen or compensate for challenges in memory, attention, problem-solving, and language.
Here’s how speech therapy can support those with MCI:
Memory Strategies
Learn proven techniques to retain and retrieve information more effectively—whether it’s remembering names, appointments, or daily routines.
Executive Functioning Support
Therapists can help with planning, organizing, time management, and setting up systems that simplify daily life.
Language & Communication Practice
Struggling to find the right words? SLPs provide exercises and strategies to support smoother, clearer communication.
Compensatory Techniques
We teach tools like:
Memory notebooks
Digital reminders
Visual schedules
Note-taking systems
These help reduce stress and increase independence.
Caregiver Support
We also work with family members to ensure they understand how to support—not overstep—and to reduce frustration on both sides.
Lifestyle Changes That Support Brain Health
While therapy is powerful, daily habits matter too. If you’ve been diagnosed with MCI or are concerned about early signs, consider the following:
Keep Learning
Lifelong learning keeps your brain agile. Take a class, learn a language, try a new hobby.
Stay Active
Regular physical activity boosts blood flow to the brain and supports overall cognitive health.
Eat Brain-Friendly Foods
Focus on a Mediterranean-style diet—rich in leafy greens, berries, whole grains, and healthy fats.
Stay Connected
Social engagement is a brain booster. Avoid isolation. Join clubs, volunteer, or keep regular calls with loved ones.
Prioritize Sleep
Sleep isn’t just rest—it’s brain maintenance. Aim for 7–9 hours per night and address any sleep disorders.
When to Seek Help
You don’t need to wait for a formal diagnosis to get support. If you or someone close to you is:
Struggling to keep up with conversations
Forgetting important things regularly
Seeming more withdrawn or confused
…it's worth having a conversation with a specialist.
You’re Not Alone—and There Is Help
Cognitive decline is scary. It can feel like losing part of yourself. But early action can slow progression, improve daily functioning, and restore confidence.
At Anywhere Speech & Language, we work with individuals and families navigating these changes every day. Whether you’re newly diagnosed, seeing early signs, or recovering from a brain injury, we’re here to help you live fully and independently for as long as possible.
Because communication is life—and we believe in your ability to adapt, grow, and thrive.
Interested in a cognitive screening or want to talk to a speech-language therapist? Contact us today to schedule a free consultation.